Acute abdomen refers to previously undiagnosed pain that arises suddenly having duration of 7 days (mostly less than 48 hours) and usually needs immediate surgical intervention.
Causes according to age
- Neonates: Intestinal atresia and stenosis, meconium ileus, meconium peritonitis, imperforate anus, annular pancreas
- Infants: Intussusception, Volvulus, Meckel’s diverticulitis
- Children: Round worm infestation, Appendicitis, Mesenteric lymphadenitis
- Adults: Appendicitis, Meckel’s Diverticulitis, Perforation of peptic ulcer, Acute Cholecystitis, Acute pancreatitis
- Elderly: Sigmoid volvulus, Intestinal obstruction from malignant growth, diverticulitis
History
Time of onset
- Pain starts early in the morning → Acute appendicitis
Mode of onset
- Sudden: Perforation, colic, volvulus and torsion
- Gradual: Obstruction
Referred pain:
- T5 to T8 → foregut → Epigastric pain
- T9 to T10 → midgut → umbilical pain
- T11, 12 L1, 2 → Hindgut → Suprapubic pain
- shoulder pain → Referred from diaphragm
- shoulder pain → Referred from spleen (Kehr’s sign)
- Kidney and ureter → Loin to the groin, inner thigh and testis
- Biliary colic → Referred to Inf. angle of Rt. shoulder
Note: For differentiating diaphragmatic pain in rt. shoulder from local pain, the leg end of the bed of pt. is raised by about 18 inches. If irritant to diaphragm is present, gravitation under diaphragm with exaggeration of pain occurs
Character
- Colicky pain: Lumen obstruction
- Burning pain: Peritonitis (Often in perforated PU)
- Severe agonizing pain: Pancreatitis and torsion
- Throbbing pain: Inflammation (Cholecystitis, Hepatitis)
Change of character of the pain
- Colicky pain to continuous pain
- Obstruction → Strangulation (Localised pain)
- Obstruction → Peritonitis (Generalised pain)
- iliac fossa pain to diminishing pain
- Most likely perforation of Gangrenous appendix
- Diminishing acute epigastric pain
- Peptic ulcer perforation entering 2nd stage
Site of Pain
Epigastric Pain
- Acute MI: difficulty breathing, sweating, nausea, radiation
- Acute pancreatitis: radiating to back, often severe, relieved by sitting up or leaning forward
- Peptic Ulcer Disease: long history of on/off symptoms, often localizes to right or left hypochondrium
- GERD: heartburn, regurgitation and dysphagia
- Gastroparesis: nausea, vomiting, early satiety, postprandial fullness, bloating
Right Upper Quadrant Pain
- Biliary colic : dull, nausea, vomiting, sweating, generally >30 minutes, plateauing within an hour, referred to Inf. angle of right scapula
- Acute cholecystitis: > 4 to 6 hrs, fever, abdominal guarding, Murphy’s sign
- Acute Cholangitis: fever, jaundice, RUQ pain
- Acute Hepatitis: jaundice, fatigue, malaise, anorexia, pale stools, dark colored urine
- Liver abscess: high grade fever, diarrhea
Left Upper Quadrant Pain
- Splenomegaly: Discomfort, Left shoulder pain, Early satiety
- Splenic infarct: Severe pain
- Splenic abscess: Fever, LUQ tenderness
- Splenic rupture: h/o Trauma, LUQ or left chest pain or left shoulder pain that worsens with inspiration
Lower Abdominal Pain
- Acute Appendicitis: Pointing sign, Rebound tenderness, nausea, vomiting, anorexia
- Diverticulitis: LLQ pain
- Nephrolithiasis: mild to severe flank pain
- Pyelonephritis: dysuria, frequency, urgency, hematuria, fever, chills and rigor, renal angle tenderness
- Acute urinary retention: Suprapubic pain
- Cystitis: Suprapubic pain, frequency, urgency, dysuria, hematuria
- Infectious Colitis: Diarrhea, may present with perforated bowel
Exaggerating and Relieving factors
- Pressure:
- Colic: relieved by pressure
- Inflammation: Exaggerated by pressure
- Deep inspiration and coughing:
- Diaphragmatic pain
- Strangury:
- During act of micturition, mostly in cystitis
- Posture:
- Relieved by Sitting forward → Pancreatitis
- Exaggerated by leaning back → Pancreatitis
- Exaggerated by movements and relieved by still → Peritonitis
- Fatty food:
- Exaggeration: Cholecystitis and pancreatitis
- Food:
- Exaggeration: Gastric ulcer
- Relief of pain: Duodenal ulcer
- Vomiting:
- Relieved in Peptic ulcer disease
- Vomiting temporarily relieves pain that again reappears immediately in Colic
- Purgatives: Appendicitis
- Straining: Perforation
Vomiting
Projectile:
- High Intestinal obstruction/ GOO
- Toxic Enteritis
Non- projectile:
- Gastroenteritis, Pancreatitis, Cholecystitis, Hepatitis, Lower Intestinal Obstruction
Vomitus:
- Intestinal Obstruction
- Firstly: Stomach content
- Then: Bilious
- Lastly: Feculent
- Biliary colic: Bilious
- PUD: Gastric content with some blood
- Gastro-colic fistula: True fecal
- Peritonitis later stages: Brown (Due to blood mixed with fecal matter)
Bowel Habit
Absolute constipation: No fecus or flatus
- Intestinal obstruction and peritonitis
Pelvic appendicitis → pelvic abscess → rectal irritation → straining during defecation → No passage of stool, but only mucus and blood → “Tenesmus”
Micturition
Strangury → painful contracting bladder during micturition even if there is no urine
- Mainly due to stones in bladder or lower ureter
A Retrocaecal or pelvic appendicitis, by irritation of urinary tract or bladder may cause this symptom and even cause hematuria misleading the clinician
Examination
Inspection
- Hernial Orifice
- Skin:
- In acute hemorrhagic peritonitis → ‘Grey Turner’ and ‘Cullen sign’
- Respiratory movement:
- Reduced movement of abdominal wall → Peritonitis
Palpation
- Tenderness
- Rebound Tenderness (Blumberg’s or release sign)
- Murphy’s test
- Muscle Guarding
- Palpation of Hernial sites
- Muscle Guarding:
- Best demonstrated by two hands with upper hand used to press and lower to feel (Gentle nature of palpation by this method reduces the chance of voluntary rigidity)
- Differentiating between thoracic and abdominal disease
- Sometimes thoracic pain can appear to be abdominal. In such cases, following can be done to distinguish between these two:
- No abdominal tenderness is present in thoracic disease. Still voluntary rigidity can be done by pt. in thoracic disease. To separate them, palpate the rigidity during expiration.
- If it is absent→ Thoracic dz
- If present → Abdominal dz
- Compression of lower thorax from side to side will cause tenderness in thoracic dz but not abdominal dz.
- No abdominal tenderness is present in thoracic disease. Still voluntary rigidity can be done by pt. in thoracic disease. To separate them, palpate the rigidity during expiration.
- Sometimes thoracic pain can appear to be abdominal. In such cases, following can be done to distinguish between these two:
- Carnett’s sign– Increased tenderness when abdominal wall muscles are contracted.Distinguishes abdominal wall pain from visceral pain
- Murphy’s sign– Patient abruptly stops a deep inspiration during palpation of the right upper quadrant. Useful in some patients with suspected cholecystitis, but its sensitivity may be diminished in the elderly
- Obturator sign– Pain elicited during passive internal rotation of flexed right thigh. Patient with a pelvic appendix may have a positive sign
- Psoas sign-Pain elicited during passive extension of rt hip when patient on lt side. Patient with a retrocecal appendix may have a positive sign
- Rovsing’s sign– Pain in rt lower quadrant during palpation of lt lower quadrant.
Percussion
- Fluid thrill: 1000-1500 ml
- Shifting dullness: 500 ml
- Puddle’s sign: 120 ml
- USG and CT: 120 ml
- Diagnostic tap: 10-20 ml
- Obliteration of liver dullness: Done in rt. mid-axillary line: for DU perforation
Auscultation
- Normal: 5-15 sounds per minute
- Silent Abdomen → Pathognomic for diffuse peritonitis and paralytic ileus
- Noisy abdomen → Acute Intestinal obstruction
Investigation
- ECG: to rule out Myocardial Infarction
- CBC: raised in case of acute appendicitis and acute cholecystitis
- Urine RE/ME: ketones (DKA), microscopic hematuria (nephrolithiasis)
- Serum electrolytes, urea and creatinine
- LFT: acute hepatitis, acute cholangitis, cholelithiasis and choledocholithiasis
- Serum amylase and lipase: Acute pancreatitis
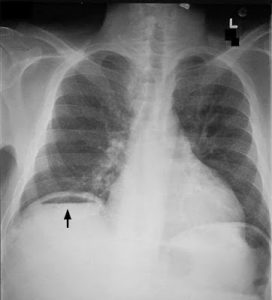
- X-ray abdomen: Erect to look for gas under diaphragm, erect and supine in case of obstruction, renal, ureteric or bladder stones (KUB)
- USG abdomen: Cholelithiasis, Pancreatitis, stones in KUB
- CT scan to confirm equivocal cases
-

Management
- Pain relief:
- Analgesics:
- Inj Ketorolac 30 mg IV
- Inj Tramadol 50 mg IV
- Antispasmodics:
- Inj Hyoscine 20 mg IV
- Analgesics:
- PPIs:
- Inj Pantoprazole 40 mg IV
- Fluid and electrolyte balance should be maintained by Ringer’s Lactate infusion.
- Antibiotics are used in cases like acute cholangitis, bowel perforation.
- Inj Ceftriaxone 1 gm IV stat
- Inj Metronidazole 500 mg IV stat
- Aspiration of gastric contents and NPO in acute pancreatitis.
- Fluid replacement, Insulin and potassium supplementation in case of DKA.
- Appendectomy for Acute Appendicitis.
- Laparotomy for Obstructed bowel and bowel perforation.